Shugri Nour, Vivian Tseng, Navisha Weerasinghe
Image 1: The PPE Lifecycle
Since the onset of the pandemic, demand for personal protective equipment (PPE), both within and beyond the health sector has increased significantly worldwide. PPE has proven to be a valuable resource in safeguarding the public and healthcare workers from the infectious disease and preventing the transmission of the virus whilst providing safe patient care. General existing practices do not allow for the recycling of PPE, which include medical masks, respirators, face shields, gloves, and gowns, due to infection control standards. However, there is opportunity to safely recycle and repurpose these primarily plastic items.
The global demand for PPE has gone unabated since the pandemic began, resulting in a pronounced increase in production, distribution, and waste generation (Patricio Silva et al., 2020). Each month of the pandemic, it is estimated that 129 billion face masks and 65 billion gloves are used worldwide by healthcare workers and the general public. From June 2020-June 2021, an estimated 63,000 tons of COVID-19 related-PPE from Canada’s healthcare system and the general public ended up in our landfills, with a smaller portion being incinerated due to biomedical contamination. A worrisome amount of PPE waste has escaped these waste streams altogether; for instance, striking quantities of PPE have washed up along Canada's coastlines. As the pandemic continues, we are seeing surges in the use of single-use plastic by 250 to 300%. This goes beyond PPE to increased consumption of test kits including swabs and plastic vials.
All of this waste produces a sizable carbon footprint. One study documented that the production, distribution and waste of PPE in the National Health Service (NHS) in England during the first six months of the pandemic was approximately twice the amount of PPE consumed in the whole of 2019, and generated 106,478 tonnes of CO2e - equivalent to 64,586 homes' electricity use for one year, or approximately 244 return flights from London to New York daily. In total, PPE use during this 6 month period added an additional 1% to the NHS’ carbon burden. The vast majority of PPE’s carbon footprint arises from the production of materials (46%) and clinical waste (39%) (Figure 1).
Figure 1. PPE-associated carbon emissions.
Adapted from Rizan C, Reed M, Bhutta MF. Environmental impact of personal protective equipment distributed for use by health and social care services in England in the first six months of the COVID-19 pandemic. Journal of the Royal Society of Medicine. March 2021.
At the outset of the pandemic, as institutions scrambled to carry out measures to protect overwhelmed healthcare systems from collapse, initiatives to reduce PPE waste were not prioritized. Moreover, the pandemic had an impact on waste-reduction efforts more generally; it has stalled efforts around the world to replace some single-use devices with reusable or at least recyclable alternatives, and to implement plastic reduction policies. In Canada, for example, the national ban of single-use plastics was delayed from earlier this year to October 2021.
As time went on, there were growing calls to develop policies, programs, and innovations to safely reduce PPE waste. These calls have been met with an array of initiatives aimed at developing reusable options, implement recycling initiatives, and reducing inappropriate use of PPE through public awareness and implementation of hospital protocols to optimize use of PPE.
Last fall, the Government of Canada itself committed to funding alternative strategies, notably the creation of compostable disposable masks and respirators in their efforts to take action on plastic waste. A Calgary based company called Roswell Downhole Technologies Incorporated and a Winnipeg based company called Precision ADM both received funding to develop innovative solutions in manufacturing compostable PPE including surgical masks, respirators, and gowns. Recently, both companies have joined up to create a full range of medically certified PPE products made from crop-based biopolymers. However, they are in the process of awaiting approval by Canadian composting facilities for intake of their used PPE products. In the meantime, they have opened their operations for grand scale production of compostable surgical masks, respirators, and other PPE products.
At the University of Toronto, two members of the Temerty Faculty of Medicine have been developing a sustainable way to ensure front-line workers have secure access to PPE. The initiative, dubbed the ROSE Project, is led by Denyse Richardson, an associate professor in the Department of Medicine, and Reena Kilian, a lecturer in the Department of Family and Community Medicine. In an effort to develop a reusable mask that meets Level 1 safety criteria (the standard for low-barrier fluid exposure), they have joined forces with a textile engineer, an architect, sewing experts, a knowledge translation expert and a medical student. On top of using locally available materials, their goal is to open-source their mask design to ensure both availability and accessibility. The masks are currently in the process of laboratory testing to ensure compliance of international safety standards.
The Children’s Hospital of Eastern Ontario (CHEO) Research Institute discovered the potential of reusable masks for decreasing PPE-related waste based on hospital staffing. Dr. Richard Webster, a clinical researcher at CHEO who has helped spearhead the initiative, described its main impetus as such: “From our hospital’s COVID screening tool we were surprised that at the moment, 60% of staff are on site for non-direct patient care. This was much higher than we expected!” Because staff who are not directly involved with patients do not require the same level of PPE as those who are, the CHEO team worked with a local charitable organization to developed a reusable cloth mask. The reusable mask, which was piloted with high satisfaction amongst staff, underwent testing at the National Research Council and has an initial particle infiltration efficiency of 88 percent, decreasing to between 72 and 77 percent after approximately 50 washes. This exceeds recommendations issued in February 2021 by the American Society for Testing Materials (ASTM) where it is indicated that high-performing or Level 2 consumer masks should meet or exceed 50 percent particle filtration efficiency (PFE) when tested. These standards from ASTM, including ones for surgical and N95 masks, are also adopted by Health Canada. This mask has now been launched as a community mask for purchase and once funding permits, the CHEO team will perform Health Canada medical device testing to approve its use in healthcare settings. The introduction of this reusable mask in healthcare settings offers a unique solution to mitigate PPE waste.
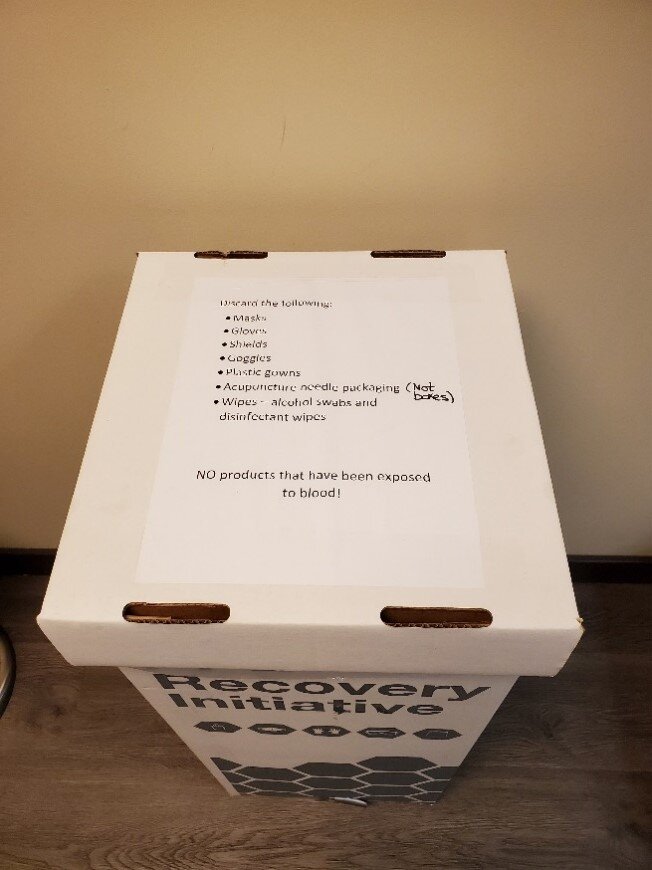
In February 2021, Canada’s first recycling program for PPE was launched in long term care and urgent care facilities across Vancouver. Recycling bins collect single-use face masks and N95 respirators from front-line workers, which are then broken down and re-purposed into construction materials. To respond to the demand for PPE recycling, TerraCycle has also created the Safety Equipment and Protective Gear Zero Waste Box, a recycling service for discarded nitrile and latex gloves, dust masks, garments, hairnets, and safety glasses. The collected waste is mechanically separated into fibers and plastic components, which can be recycled, composted, or turned into new plastic products. More general PPE recovery programs, such as the PPE Recovery Initiative launched by RecycleSmart and Green Circle Ideas earlier this year, have made PPE collection accessible to a broader audience of allied health professionals and Canadian businesses in general.
Images 2 & 3: PPE Recovery Initiative receptacles at a Toronto Massage Therapy office.
COVID-19 remains a major threat to public health, and our response is contributing to the ongoing threat of significant environmental harms associated with the increased usage of PPE. Given proper design standards, material selection, and user guidelines, reusable PPE has been shown to be effective in infection control while providing a suitable environmentally friendly alternative. For example, a UK study identified that over a six-month period the use of reusable gowns and face shields could have saved 20% of the total emissions from disposable PPE. Another factor that may decrease carbon emissions is the local production of PPE supplies. In fact, domestic manufacturing in the United Kingdom would reduce 12% of the emissions from PPE by limiting airfreight use and saving 12,491 tonnes CO2e over the six-month study period. This reduction was seen due to the elimination of greenhouse gases produced from overseas travel. As a result, the UK study demonstrates how other countries can limit their emissions as well by prioritizing cleaner energy used in domestic manufacturing of PPE.
Canada and our healthcare system face many challenges up ahead as we move towards net-zero carbon while continuing to curb the spread of COVID-19. Considering that the usage and demands for PPE are only expected to grow around the world, the need for our healthcare system to scale down this impact and invest in alternative, innovative strategies cannot be understated. In this way, COVID-19 was the primary catalyst for short-term and long-term changes in plastic waste management systems and technologies.
About the authors
Shugri Nour is a Registered Nurse working in Hemodialysis for 5 years. She completed her Master of Nursing (MN) at U of T. Shugri is currently a Research Assistant at the Centre for Sustainable Health Systems where she is involved in developing content on sustainable food in healthcare.
Vivian Tseng (BHsc) is a second year Master of Public Health (MPH) student at the Dalla Lana School of Public Health, University of Toronto. She holds a bachelor's degree in Psychology and Health Studies from the University of Toronto. Vivian is interested in health equity, specifically how to shape policies and programs to ensure equitable access to the social determinants of health necessary to improve population health outcomes.
Navisha Weerasinghe is a Registered Nurse working in the Emergency Department and Med/Surg units in GTA hospitals. Navisha recently completed her Master of Nursing (MN) - Clinical program at the University of Toronto. Navisha is currently a Research Assistant with the Centre for Sustainable Health Systems. Her interests include greening healthcare systems and finding innovative solutions to reduce ward waste in healthcare settings.
All CSHS guest posts are published under the CreativeCommons Attribution Non-commercial Share Alike license. Guest Contributors are free to publish their guest posts elsewhere.
If you’ve got an idea for a blog post you’d like to author, please contact us.